Overview
ADHD and autism are both neurodevelopmental conditions. They frequently co-occur, and when they do, the combined presentation is often referred to as AuDHD. While AuDHD is not a separate diagnosis, it is a useful term for describing the lived experience of having both ADHD and autism.
There is considerable misunderstanding and misinformation about ADHD, autism, and how they interact. This article aims to provide a clear, clinically grounded overview of both conditions, explain how they overlap, and highlight why combined presentations are often missed. The intention is to help readers feel more confident and better informed, and able to recognise traits in themselves or others.
Key points:
- ADHD and autism are lifelong neurodevelopmental conditions.
- They often co-occur.
- Overlapping traits can create a complex and sometimes confusing presentation.
- Understanding these overlaps can support self-acceptance and access to appropriate support.
Neurodevelopmental Conditions: A Shared Framework
ADHD and autism are described as neurodevelopmental disorders, meaning they:
- Often appear in early childhood.
- Affect brain development and processing.
- Influence functioning across the lifespan.
Neurodevelopmental conditions can impact:
- Communication.
- Learning.
- Movement.
- Relationships.
They can affect multiple areas of life, including:
- Personal life.
- Education.
- Work.
- Friendships.
For some individuals, traits are evident early in childhood. For others, difficulties become more noticeable in adulthood, often due to increased demands such as full-time work, relationships, parenting, and reduced capacity to rely on earlier coping strategies.
ADHD: A Clinical Overview
What Is ADHD?
Attention Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental condition characterised by differences in attention regulation, activity levels, and impulse control.
- Worldwide prevalence in children: estimated at approximately 5%.
- Adult prevalence: affects around 3–4 in every 100 adults.
- ADHD is highly heritable: ADHD is more common in people who have a sibling or close family member with ADHD.
- It is a lifelong condition for many people, though presentation can change over time.
ADHD commonly co-occurs with other mental health conditions, particularly anxiety and depression.
Core Symptom Domains in ADHD
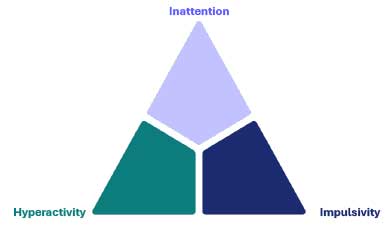
Clinicians assess ADHD across three core domains:
- Inattention
- Hyperactivity
- Impulsivity
Individuals may show traits across all three domains (combined presentation) or predominantly within one.
Inattention
Common inattentive traits include:
- Difficulty sustaining attention (e.g. zoning out in meetings).
- Needing to reread information multiple times.
- Difficulty initiating tasks or completing them consistently.
- Making avoidable mistakes in school or work.
- Disorganisation, forgetfulness, and frequently losing items.
Clinicians assess how persistent these traits are and how significantly they impact daily functioning.
Hyperactivity
Hyperactivity in adults may differ from childhood presentations.
Rather than overt physical restlessness, it often includes:
- Internal restlessness.
- Racing or intrusive thoughts.
- Difficulty relaxing, particularly in the evening.
- Feeling constantly ‘on the go’.
In conversation, hyperactivity may present as:
- Interrupting due to fear of forgetting what they want to say.
- Rapid or pressured speech.
Impulsivity
Impulsivity may involve:
- Making decisions without fully considering consequences.
- Impulsive spending.
- Risk-taking behaviours, such as taking drugs or alcohol.
- Difficulty waiting in queues or for delayed outcomes.
These traits are assessed in context and across different areas of life.
Diagnosing ADHD and autism – general principles
International diagnostic criteria, e.g. DSM-5 and ICD-11 are centred on:
- Presence of traits across the three core domains.
- Evidence of symptoms from childhood.
- Impact of symptoms on day-to-day functioning.
- Ruling out other possible conditions.
The assessment process typically includes:
- Completing a self-report questionnaire.
- An informant questionnaire (ideally completed by someone who you’ve known since childhood).
- A detailed clinical interview.
International diagnostic criteria (e.g. DSM-5 and ICD-11) are centred on:
ADHD Post-Diagnosis Care Principles
If you are diagnosed with ADHD, there are treatments. Treatment is most effective when part of a comprehensive support plan.
This may include:
Medication
- Stimulant or non-stimulant medications.
- Used alongside, not instead of, other supports.
Psychological and behavioural interventions
- ADHD-specific CBT.
- Coaching approaches.
Education and reframing
- Educating yourself about ADHD, its symptoms and how they impact you.
- Focussing on strengths, identity and self-acceptance.
Lifestyle factors
- Adequate and regular sleep.
- Regular physical activity.
- Balanced nutrition.
Autism Spectrum Disorder: A Clinical Overview
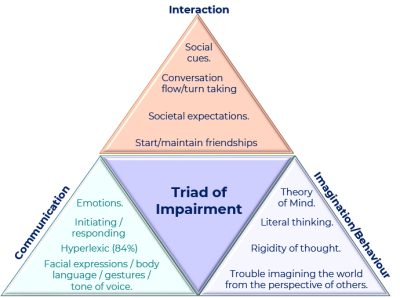
Core Diagnostic Areas (Triad of Impairment)
Whilst in ADHD you could have all three types or some of them, in autism, clinicians look for symptoms across all three areas below to meet the criteria.
- Social communication.
- Social interaction.
- Restricted, repetitive patterns of behaviour or interests.
Social Communication
Social communication is everything to do with giving and receiving messages. In autism, there are difficulties in that transaction, including:
- Understanding and expressing emotions.
- Initiating and responding in conversation.
- Interpreting facial expressions, body language, and tone of voice.
- Eye contact (which may be reduced, atypical, or inconsistent).
Some autistic individuals are hyperlexic, meaning they have advanced reading or language skills alongside social communication differences.
Social Interaction
Social interaction is everything to do with engaging with one another.
Differences may include:
- Difficulty interpreting social cues.
- Challenges with conversational flow and turn-taking.
- Uncertainty around social expectations.
- Difficulty initiating or maintaining friendships.
Imagination, Thinking and Behaviour
This domain includes:
- Theory of mind.
- Literal thinking.
- Rigidity of thought.
- Difficulty imagining situations from another person’s perspective.
- Repetitive behaviours or highly focused interests.
Alexithymia
Alexithymia is a term which describes people who struggle to identify their own emotional states and those of others.
Struggling to identify emotions:
- General population: 10%.
- Autistic individuals: 40–50%.
Alexithymia can significantly affect emotional regulation and mental health.
Masking
Masking involves consciously or unconsciously altering behaviour to appear non-autistic. This may be in the form of masking facial expressions or body language. You may see children developing interests that their peers have to avoid standing out and be vulnerable to bullying.
Masking = changing how you act to blend in.
Examples include:
- Hiding natural reactions.
- Copying others’ social behaviour.
- Trying to avoid judgement or rejections, at school, work, home and socially.
- Adopting socially acceptable interests.
Long-term effects of masking can lead to mental health impacts in the form of anxiety and low self-esteem. There is also a higher rate of delayed diagnosis if masking is at play.
Masking can lead to:
- Anxiety and low self-esteem.
- Delayed diagnosis.
- Autistic burnout.
- Exhaustion from continual self-monitoring.
Diagnosing Autism
The diagnostic process follows the same principles as for ADHD.
Diagnosis involves a combination of methods, including:
- Early developmental history.
- Informant and self-report questionnaires.
- Clinical assessment via interview.
As with ADHD, autism is present from childhood, even if identified later in life.
There will usually be an outcome at the end of the assessment, but in some rare cases, another review may be needed.
After a Diagnosis
After a diagnosis, it’s very important to educate yourself around what autism looks like, because it looks very different in each individual. It’s also important to recognise – and treat – any other mental health conditions alongside autism, such as depression, anxiety or ADHD.
Understanding and accepting your difficulties, and putting measures in place – in education or the workplace – is key to living well as an autistic individual.
What a Good Treatment Plan Looks Like
- Treat any co-occurring conditions.
- Person-centred and strength-based.
- Individualised – takes into account sensory, communication and cognitive profiles.
- Collaborative – involves the autistic person and, where appropriate, family and carers.
- Neuro-affirming.
- Trauma-informed, recognising the high rates of adverse experiences.
- Focused on quality of life with making reasonable adjustments in environment, workplaces and communication.
Good psychosocial support is autism-affirming .. it adapts the world around the person.
AuDHD: When ADHD and Autism Co-Occur
What Is AuDHD?
AuDHD is a term that’s used to describe the combined lived experience of ADHD and autism.
- Not a separate diagnosis.
- A clinically recognised co-occurrence.
- Traits that may conflict or complement each other.
- A unique neurodevelopmental presentation.
Before diagnostic criteria changed in 2013, when the DSM-5 was introduced, individuals could not be formally diagnosed with both conditions. Clinicians would only make the diagnosis that showed more prominent symptoms. This has contributed to under-recognition.
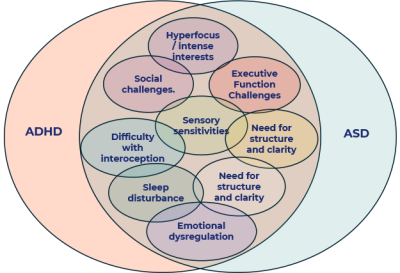
Overlapping Traits in AuDHD
AuDHD is a unique neurodevelopmental experience in which traits can really conflict with each other at times, but at the same time also complement each other. Individuals may feel really confused about what’s going on, because sometimes they may find themselves in one presentation; at other times it may look different.
Common overlapping features include:
- Hyperfocus and intense interests.
- Executive functioning difficulties.
- Sensory sensitivities.
- Social communication challenges.
- Emotional dysregulation.
- Sleep disturbance.
- Need for clarity and structure.
Why is it often missed?
The combined diagnosis is often missed due to:
- Symptom overlap.
- Masking.
- Internalised presentations – a lot of emotional impact that is not visible to others.
Core Traits in AuDHD: Interacting Symptoms
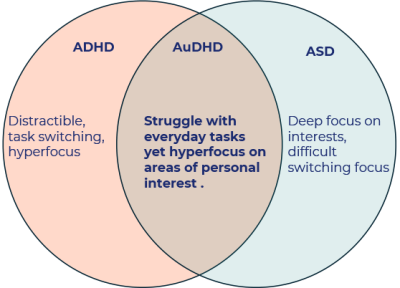
Attention and focus
- ADHD: Distractibility, task-switching, hyperfocus.
- Autism: Deep focus on interests, difficulty switching focus.
- AuDHD: Struggle with everyday task, yet hyperfocus on areas of personal interest.
The ADHD would make the individual easily distractible, for example, struggling to do day-to-day tasks. But there will be periods of intense hyperfocus where they are able to focus for long periods of time in an area of interest.
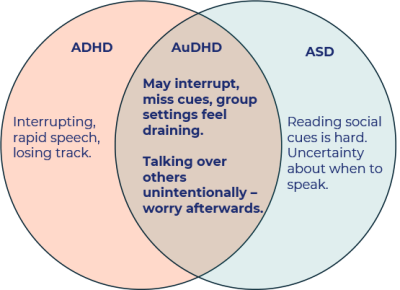
Social communication
- ADHD: Impulsive speech, interrupting, losing track.
- Autism: Difficulty reading social cues, uncertainty about when to speak.
- AuDHD: Unintentional conversational dominance followed by self-reflection or worry. May interrupt, miss cues, group settings feel draining.
Often an individual will say: “I was engaged and enthusiastic, but afterwards I realised I ended up taking over the conversation.” This can take an emotional toll on people wondering about how they should have presented themselves.
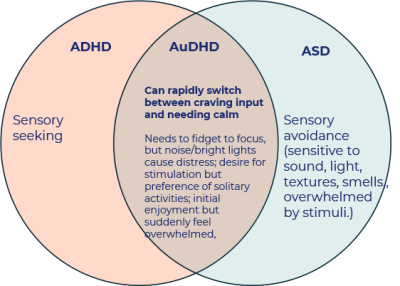
Sensory processing
- ADHD: Sensory seeking.
- Autism: Sensory avoidance (sensitivity to sound, light, textures, smells, overwhelmed by stimuli).
- AuDHD: Rapid shifts between craving stimulation and needing calm. Needs to fidget to focus, but noise/bright lights cause distress; desire for stimulation but preference for solitary activities; initial enjoyment, but suddenly feeling overwhelmed.
This can fluctuate, not only day-to-day, week to week, but even hour to hour, which can create quite a lot of confusion for the individual experiencing it.
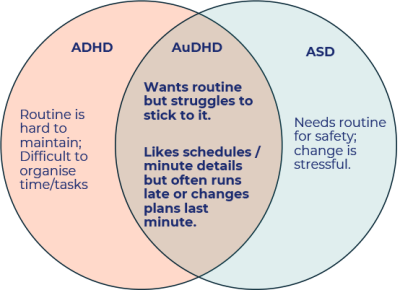
Routine and flexibility
- ADHD: Difficulty maintaining routines, difficult to organise time/tasks.
- Autism: Reliance on routine for safety, change is stressful.
- AuDHD: Strong desire for structure but difficulty sticking to it. Likes schedules, minute details, but often runs late or changes plans at the last minute.
Individuals with ADHD find it hard to maintain routine, whereas autistic people find safety in routine. How this would present with AuDHD is really wanting to have and keep to a routine, but struggling to sustain it.
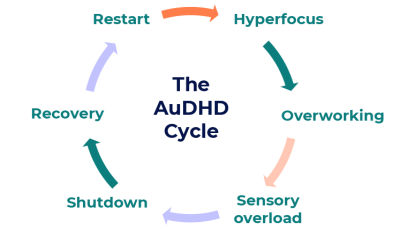
The AuDHD Burnout Cycle
It’s really important to think about burnout in a combined diagnosis.
A commonly reported pattern:
Hyperfocus → Overworking → Sensory overload → Shutdown → Recovery → Restart
Understanding this cycle can help individuals plan rest, pacing and preventative strategies.
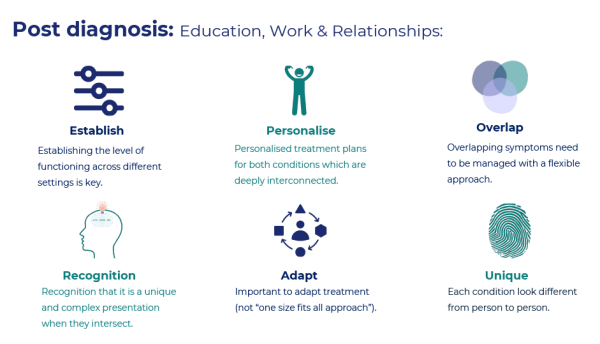
Diagnosis and Support in AuDHD
- ADHD and autism are currently assessed separately.
- One condition may mask the other.
- Presentations are often nuanced rather than clear-cut.
Diagnosis can provide validation, access to support, and a framework for self-understanding.
Once you have the diagnosis, it’s really about educating yourself about what the combined presentation looks like. As we have seen in this article, there can be quite a lot of mixed messages, and it’s really important to filter through what the presentation looks like for you.
The overlapping symptoms can cause a lot of confusion, so make sure you communicate this to family members.
It’s important to treat the ADHD, maybe with medication, but it’s also about treating any of the comorbid conditions you may have, such as anxiety and depression.
It’s really important to have a personalised and adaptive plan. This should be:
- Individualised.
- Flexible.
- Strength-based.
- Focused on quality of life.
Reasonable adjustments in education and employment are central to enabling individuals to function at their best.
Support and Treatment Pathways
Moving Forward
Understanding AuDHD is a process. Education, self-reflection, and appropriate support can significantly improve wellbeing and functioning.
Resources and where to get help
If you identify with symptoms and you would like an assessment, you need to request a referral via your GP.
Other helpful resources include:
- ADHD UK.
- National Autistic Society.
- Local care teams (speak to your GP).
Key message: You are not alone! Support is available.
Gaining understanding of your neurodevelopmental profile is a meaningful step towards self-acceptance and thriving.







Leave A Comment